Complete Heart Guide
Heart Anatomy & Structure
The human heart is a muscular organ about the size of your fist, weighing approximately 8-12 ounces. Located slightly left of center in your chest, it's divided into four chambers that work in perfect coordination to pump blood throughout your body. Understanding its structure is key to appreciating how this remarkable organ functions.
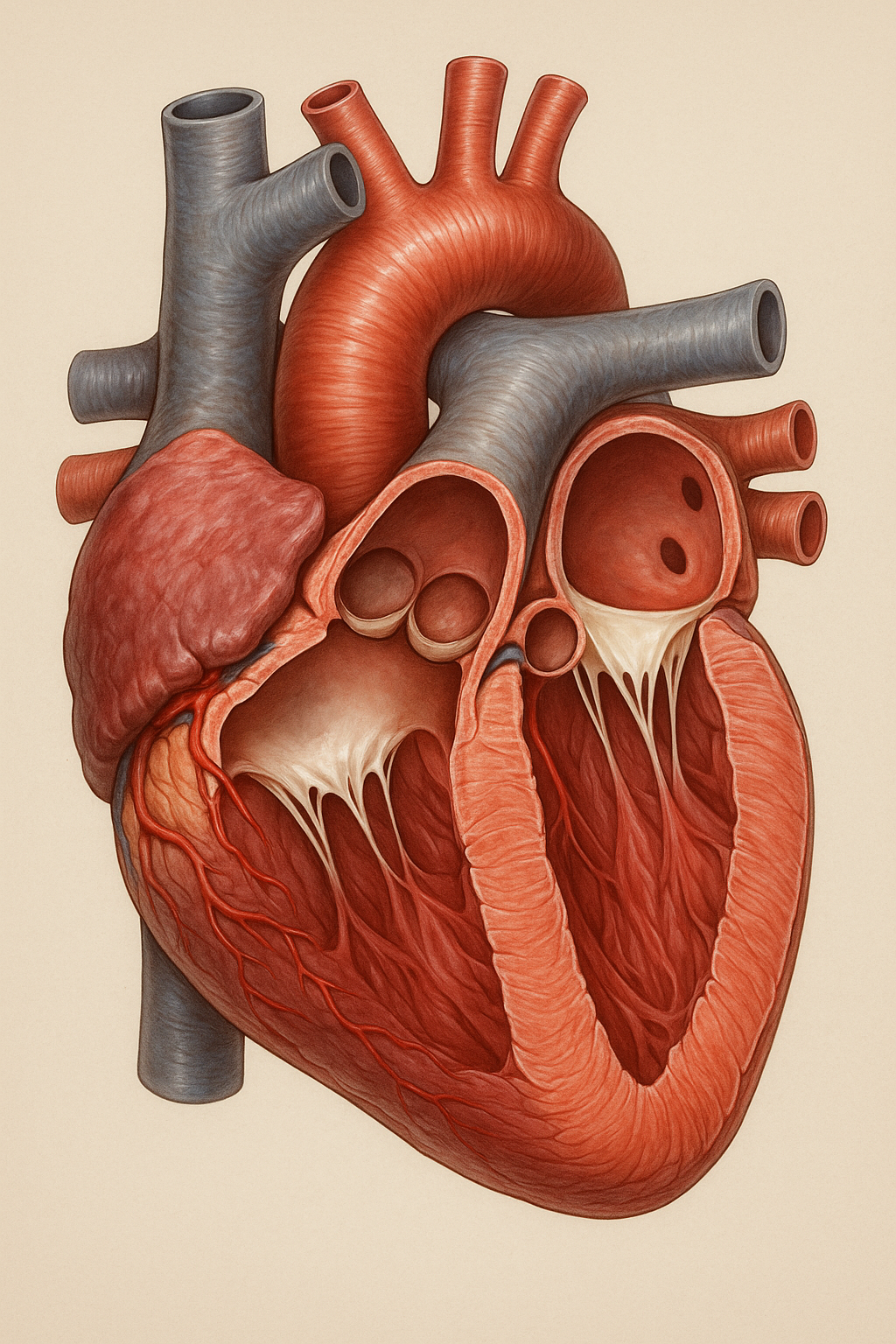
Detailed view of human heart anatomy showing the four chambers, major vessels, and valve locations. Image: Medical illustration of heart structure and components.
The Four Chambers
| Chamber | Location | Function | Receives Blood From | Sends Blood To |
|---|---|---|---|---|
| Right Atrium | Upper right | Receives deoxygenated blood | Body tissues via vena cava | Right ventricle |
| Right Ventricle | Lower right | Pumps blood to lungs | Right atrium | Lungs via pulmonary artery |
| Left Atrium | Upper left | Receives oxygenated blood | Lungs via pulmonary veins | Left ventricle |
| Left Ventricle | Lower left | Pumps blood to body | Left atrium | Body via aorta |
How Your Heart Works
Your heart is essentially a dual pump system working 24/7 to circulate blood throughout your body. The right side pumps deoxygenated blood to the lungs for oxygen pickup, while the left side pumps oxygen-rich blood to all body tissues. This continuous cycle delivers nutrients and removes waste from every cell in your body.

Visualization of blood flow through the heart showing the dual circulation system. Red indicates oxygenated blood, blue shows deoxygenated blood.
The Pumping Mechanism
Muscle Contraction Process
The heart muscle (myocardium) contracts through a coordinated electrical signal that spreads across the heart wall. This contraction squeezes blood out of the chambers. When the muscle relaxes, the chambers fill with blood again. This squeeze-and-release action happens about 60-100 times per minute at rest, and can increase to over 200 beats per minute during intense exercise.
Blood Flow Pathway
- Deoxygenated Blood Return: Blood returns from body tissues to right atrium via superior and inferior vena cava
- Right Heart Circulation: Blood flows from right atrium to right ventricle, then pumped to lungs via pulmonary artery
- Lung Oxygenation: In the lungs, blood releases carbon dioxide and picks up fresh oxygen
- Oxygenated Blood Return: Oxygen-rich blood returns to left atrium via four pulmonary veins
- Left Heart Circulation: Blood flows from left atrium to left ventricle, then pumped to body via aorta
- Systemic Distribution: Arteries branch throughout the body, delivering oxygen and nutrients to all tissues
- Venous Return: Deoxygenated blood returns via veins to complete the cycle
The Cardiac Cycle
Each heartbeat follows a precise sequence called the cardiac cycle, consisting of two main phases: systole (contraction) and diastole (relaxation). Understanding this cycle helps explain blood pressure readings, heart sounds, and the timing of cardiac events that keep your circulation flowing efficiently.
The ventricles contract forcefully, pushing blood out through the aortic and pulmonary valves. This creates the higher "systolic" pressure reading and produces the first heart sound ("lub").
The ventricles relax and fill with blood from the atria. This creates the lower "diastolic" pressure reading and produces the second heart sound ("dub") when valves close.
S2 ("Dub"): Closure of aortic and pulmonary valves at end of systole
Additional sounds may indicate valve problems or other cardiac issues.
Diastolic Pressure: Lowest pressure during ventricular relaxation (bottom number)
Normal: 120/80 mmHg or lower
Cardiac Output
Heart's Pumping Capacity
Cardiac Output = Heart Rate × Stroke Volume
A healthy heart pumps about 5-6 liters of blood per minute at rest. Stroke volume (amount pumped
per beat) is typically 60-80ml. During exercise, cardiac output can increase 4-5 times through
increased heart rate and stroke volume to meet increased oxygen demands.
Heart's Electrical System
Your heart has its own electrical system that controls the timing and coordination of each heartbeat. This intricate network ensures that the chambers contract in the proper sequence to maintain efficient blood flow. Understanding this system helps explain heart rhythm disorders and the importance of regular, coordinated electrical activity.

Illustration of the heart's electrical conduction system showing the pathway of electrical impulses that coordinate each heartbeat.
Located in the right atrium, the SA node generates electrical impulses 60-100 times per minute. It sets your heart's natural rhythm and adjusts rate based on your body's needs through nervous system input.
Located between atria and ventricles, the AV node delays the electrical signal briefly, allowing the atria to empty completely before the ventricles contract. Acts as a backup pacemaker if the SA node fails.
Carries electrical signals from the AV node down the septum and branches to left and right ventricles. Ensures coordinated contraction of both ventricles for efficient blood pumping.
Spread throughout the ventricular walls, these fibers ensure that the electrical signal reaches all areas of the ventricles simultaneously, creating coordinated, powerful contractions.
Electrocardiogram (ECG/EKG)
Reading Your Heart's Electrical Activity
An ECG records the electrical activity of your heart through electrodes placed on your skin. The characteristic pattern shows P waves (atrial depolarization), QRS complex (ventricular depolarization), and T waves (ventricular repolarization). Abnormal patterns can indicate rhythm disorders, heart damage, or other cardiac conditions.
Blood Circulation Pathways
Your cardiovascular system consists of two main circulation loops: pulmonary circulation (heart to lungs) and systemic circulation (heart to rest of body). These pathways work together to ensure every cell receives oxygen and nutrients while removing waste products. Understanding these pathways helps appreciate how heart problems can affect your entire body.
Right ventricle → Pulmonary arteries → Lung capillaries → Pulmonary veins → Left atrium. This shorter circuit handles gas exchange, releasing CO₂ and picking up O₂. Lower pressure system (25/10 mmHg) suitable for delicate lung tissues.
Left ventricle → Aorta → Arteries → Capillaries → Veins → Vena cava → Right atrium. This longer circuit delivers nutrients and removes waste from all body tissues. Higher pressure system (120/80 mmHg) to reach distant organs.
Left and right coronary arteries branch from the aorta to supply the heart muscle itself. The heart receives about 5% of cardiac output but extracts 70% of available oxygen due to its high metabolic demands. Critical for heart function.
The brain receives about 15% of cardiac output through carotid and vertebral arteries. Special autoregulation maintains constant blood flow despite pressure changes. The blood-brain barrier protects delicate brain tissue from toxins.
Vascular System Components
- Arteries: Thick-walled vessels carrying blood away from heart under high pressure
- Arterioles: Small arteries that regulate blood flow to specific tissues
- Capillaries: Microscopic vessels where gas and nutrient exchange occurs
- Venules: Small veins that collect blood from capillaries
- Veins: Thin-walled vessels returning blood to heart, equipped with one-way valves
- Lymphatic System: Parallel system that returns tissue fluid and fights infection
Factors Affecting Heart Health
Your heart health is influenced by a complex interplay of genetic, lifestyle, environmental, and medical factors. While you cannot change your genetics or age, many heart disease risk factors are modifiable through lifestyle choices. Understanding these factors empowers you to take proactive steps to protect your cardiovascular health.
Non-Modifiable Risk Factors
Modifiable Risk Factors
Affects 45% of adults. Forces heart to work harder, damages arteries. Goal: <130/80 mmHg. Manageable through diet, exercise, weight loss, stress reduction, and medication when needed.
LDL "bad" cholesterol builds up in arteries. Total cholesterol goal: <200 mg/dL. Improved through diet changes, regular exercise, weight management, and statins when prescribed.
Increases heart disease risk 2-4 times. Damages blood vessels, reduces oxygen, promotes clotting. Benefits of quitting begin within 20 minutes and continue for years.
Doubles heart disease risk through blood vessel damage. Good glucose control (HbA1c <7%) significantly reduces complications. Managed through diet, exercise, monitoring, and medication.
Excess weight increases heart workload and raises blood pressure. BMI >30 significantly increases heart disease risk. Even 5-10% weight loss provides substantial health benefits.
Sedentary lifestyle doubles heart disease risk. Just 150 minutes of moderate exercise weekly reduces risk by 30-35%. Any movement is better than none - start small and build gradually.
Chronic stress increases cortisol, inflammation, and blood pressure. Linked to heart attacks and arrhythmias. Manageable through meditation, exercise, social support, and stress reduction techniques.
Moderate consumption may benefit heart health, but excess increases blood pressure, heart failure risk, and arrhythmias. Limit: 1 drink/day for women, 2 for men.
Common Heart Problems
Heart diseases affect millions of people worldwide and are the leading cause of death globally. Understanding common heart conditions helps you recognize symptoms early and seek appropriate treatment. Many heart problems are preventable and treatable when caught early.

Medical illustration showing various heart conditions and their effects on cardiac structure and function.
Plaque buildup narrows coronary arteries, reducing blood flow to heart muscle. Can cause chest pain (angina), heart attacks, and heart failure. Preventable through lifestyle changes and treatable with medications, procedures, or surgery.
Occurs when coronary artery becomes completely blocked, killing heart muscle. Symptoms include chest pain, shortness of breath, nausea, sweating. Time is muscle - immediate treatment saves lives and prevents permanent damage.
Heart muscle becomes weak or stiff, unable to pump blood efficiently. Causes fatigue, shortness of breath, swelling. Can result from CAD, high blood pressure, or other conditions. Manageable with medications and lifestyle changes.
Heart beats too fast, too slow, or irregularly. Can range from harmless to life-threatening. Atrial fibrillation increases stroke risk. Symptoms include palpitations, dizziness, chest pain. Many treatable with medications or procedures.
Heart valves don't open or close properly, disrupting blood flow. Can be congenital or acquired through aging, infection, or other diseases. May cause fatigue, shortness of breath, chest pain. Often repairable or replaceable surgically.
Heart muscle becomes enlarged, thick, or rigid. Can be genetic, caused by infections, alcohol, or unknown factors. May lead to heart failure or sudden cardiac death. Treatment focuses on managing symptoms and preventing complications.
Heart Disease Prevention Strategies
The best treatment for heart disease is prevention. Up to 80% of premature heart disease and strokes are preventable through lifestyle modifications. These evidence-based strategies can dramatically reduce your risk and improve your overall cardiovascular health.

Lifestyle modifications and prevention strategies for optimal heart health and disease prevention.
Focus on fruits, vegetables, whole grains, lean proteins, healthy fats. Limit sodium (<2,300mg), saturated fats, trans fats, added sugars. Include omega-3 rich fish, nuts, olive oil. Reduces heart disease risk by 30%.
Aim for 150 minutes moderate or 75 minutes vigorous exercise weekly. Include strength training 2x/week. Start slowly and gradually increase. Any activity counts - walking, swimming, dancing, gardening. Reduces heart disease risk by 35%.
Smoking cessation provides immediate and long-term benefits. Risk drops 50% within 1 year, returns to non-smoker levels in 15 years. Use nicotine replacement, medications, counseling, support groups. Avoid secondhand smoke too.
Maintain BMI 18.5-24.9, waist circumference <40" (men) or <35" (women). Focus on gradual, sustainable changes. Combine diet and exercise. Even 5-10% weight loss provides significant health benefits.
Keep blood pressure <130/80 mmHg. Regular monitoring, DASH diet, weight loss, exercise, stress reduction, limit alcohol, reduce sodium. Take medications as prescribed. Home monitoring helps track progress.
Total cholesterol <200 mg/dL, LDL <100 mg/dL (or <70 for high risk), HDL >40 (men) or >50 (women). Diet, exercise, weight loss help. Statins when indicated. Get tested every 4-6 years, more often if at risk.
Prevent type 2 diabetes through lifestyle changes. If diabetic, maintain HbA1c <7%. Regular monitoring, medication compliance, healthy diet, exercise. Diabetes doubles heart disease risk but good control reduces complications.
Poor sleep increases heart disease risk. Maintain consistent sleep schedule, dark/cool room, avoid screens before bed, limit caffeine. Address sleep apnea if present. Good sleep supports blood pressure control and heart health.
Practice relaxation techniques: meditation, deep breathing, yoga, tai chi. Exercise regularly, maintain social connections, pursue hobbies. Consider counseling for chronic stress. Stress reduction improves blood pressure and heart health.
The Power of Prevention
Following just 5 key lifestyle factors (healthy diet, regular exercise, normal weight, not smoking, moderate alcohol) can reduce heart disease risk by up to 86% and increase life expectancy by 12-14 years. Small changes compound over time to create dramatic health improvements.
Lifestyle Optimization for Heart Health
Optimizing your lifestyle for heart health goes beyond basic prevention. These advanced strategies help you achieve peak cardiovascular fitness and resilience. Focus on creating sustainable habits that support long-term heart health and overall well-being.

Optimal lifestyle choices for maximum heart health including exercise, nutrition, and wellness practices.
Advanced Nutrition Strategies
- Anti-inflammatory Foods: Emphasize foods rich in omega-3s, antioxidants, and polyphenols
- Intermittent Fasting: May improve cardiovascular risk factors when done safely
- Plant-Forward Diet: Increase vegetable and fruit intake to 8-10 servings daily
- Mindful Eating: Practice portion control and eat slowly to support weight management
- Hydration: Maintain adequate hydration for optimal blood viscosity and circulation
- Limit Processed Foods: Minimize ultra-processed foods that increase inflammation
Exercise Optimization
Environmental Factors
- Air Quality: Minimize exposure to pollution, use air purifiers indoors
- Temperature Therapy: Consider sauna use and cold exposure for cardiovascular benefits
- Nature Exposure: Spend time outdoors to reduce stress and improve mental health
- Social Connections: Maintain strong relationships and community involvement
- Purpose and Meaning: Engage in activities that provide sense of purpose
Monitoring and Tracking
Use Technology Wisely
Heart Rate Hero and similar apps can help track your cardiovascular health metrics. Monitor resting heart rate, heart rate variability, blood pressure trends, and activity levels. Use data to guide lifestyle adjustments and celebrate improvements over time.
Warning Signs to Watch
Recognizing early warning signs of heart problems can be life-saving. While some heart attacks are sudden and intense, many start slowly with mild symptoms. Learn to recognize these signs and seek immediate medical attention when necessary. Early intervention dramatically improves outcomes.

Emergency medical response and the importance of recognizing heart attack warning signs early.
Emergency Symptoms - Call 911 Immediately
• Severe chest pain or pressure lasting more than a few minutes
• Chest pain radiating to arms, back, neck, jaw, or stomach
• Sudden severe shortness of breath
• Cold sweats, nausea, or vomiting with chest discomfort
• Sudden dizziness, lightheadedness, or fainting
• Rapid or irregular heartbeat with other symptoms
Crushing chest pain, pressure or tightness in chest, pain radiating down left arm, profuse sweating, shortness of breath, nausea. Pain may feel like severe indigestion or heartburn.
Uncomfortable pressure, squeezing, or pain in center of chest. Pain or discomfort in arms, back, neck, jaw, or stomach. Shortness of breath, breaking out in cold sweat, nausea, or lightheadedness.
Palpitations, racing heart, skipped beats, chest fluttering, dizziness, fainting, shortness of breath, chest pain. Some arrhythmias are harmless, others life-threatening. Get evaluated promptly.
Shortness of breath during activity or lying down, fatigue, weakness, swelling of legs, ankles and feet, rapid or irregular heartbeat, persistent cough or wheezing with white or pink blood-tinged phlegm.
When to Seek Medical Attention
Trust Your Instincts
If something feels wrong, seek medical attention. Heart attack symptoms can be subtle and vary greatly between individuals. It's better to be cautious and get checked than to ignore potentially serious symptoms. Healthcare providers would rather see you for a false alarm than miss a real emergency.